When did they start this procedure?

The history of septoplasty began in 1757 when Dr. Quelmatz became one of the earliest physicians to address septal deformities . “Septoplasty,” derived from the Greek words septo (“pertaining to septum”) and plassein (“to shape”) is a surgery performed to achieve two results:
- To improve the breathing function of the nose by opening the airway
- To straighten the septum to the midline position, and in turn improve the cosmetic look of the nose.
Surgical septoplasties began to increase in popularity in the late 19th century when the Bosworth operation became the most common operation in the United States. The Bosworth operation was used to correct nasal obstruction caused by nasal septum deviation.
What is this procedure?
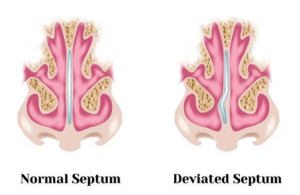
A septoplasty is the surgical correction of deformities and defects of the nasal septum; the partition between the nostrils. This is a surgical procedure that is performed in an outpatient setting and requires opening the nasal airway by removing the deviated portion, followed by reconstructing the remaining bone and cartilage. As a result, a person should experience improvement in their breathing, as well as improvement in the shape, size, and symmetry of their nose, bringing it into better proportion with the rest of their face.
Who needs this procedure?
Many may benefit from a septoplasty procedure and the indications often range. Some patients may present with a history of sinusitis, recent nasal trauma, obstructive sleep apnea, allergic rhinitis, or previous nasal surgery and they will often report symptoms of unilateral or bilateral nasal airway obstruction that is not relieved with decongestants or nasal steroid sprays. Not only do patients with a history of nasal obstruction caused by structural deformity or trauma benefit from this procedure, but it also may provide relief to those with a history of epistaxis, or nose bleeds. As a result of septal deviation, a person may experience mucosal drying and crusting, which in turn could cause intermittent epistaxis. Eliminating the deviation could resolve the issue of nosebleeds. More commonly, a septoplasty may be performed for cosmetic purposes and will often prove to be a great source of donor cartilage for rhinoplasty patients. Finally, a bit less common, but still equally as important, septoplasties may be done to provide surgical access for patients undergoing pituitary tumor resection.
Are there non-surgical treatments?
At this time, this procedure is done surgically, either with local anesthesia or under general anesthesia.
What is the surgical treatment like local or sedation?
Anesthesia Options for Septoplasty
A septoplasty may be performed under local anesthesia or general anesthesia. Each option has its advantages and disadvantages, including variations in cost, awareness, safety, and side effects. Because a septoplasty is an elective surgery, a patient will undergo a pre-operative assessment to determine anesthetic suitability. Regardless of the anesthetic option, septoplasty anesthesia is performed in conjunction with local anesthesia (lidocaine mixed with epinephrine) to numb the nose and to reduce bleeding.
Local anesthesia
Local anesthesia will numb the nasal area and is often combined with a sedative that will leave you feeling relaxed and/or groggy, without losing consciousness. Most often, the surgeon will utilize lidocaine mixed with epinephrine, which will work to numb the area and decrease overall bleeding.
General Anesthesia
Patients undergoing general anesthesia will have their respirations maintained by a ventilator. The depth of anesthesia will be adjusted as necessary to keep blood pressure low, which will in turn, minimize bruising, swelling, and bleeding. A motionless and comfortable patient with minimal bleeding will optimize operating conditions and provide more favorable surgical outcomes.
Oftentimes, the main concern that comes with the use of general anesthesia is fear of postoperative nausea and vomiting. While postoperative vomiting is not only unpleasant, when it occurs following a septoplasty, vomiting may dramatically elevate blood pressure levels leading to much heavier facial bruising, swelling, and discomfort. By combining narcotic-free general anesthesia with anti-nausea medications, the incidence of clinically significant vomiting following a septoplasty is significantly reduced and may be eliminated altogether. It is worth noting that the absence of narcotics does not necessarily equate to compromised pain control as each patient’s recovery and recovery needs are unique, with many reporting to be off of pain relievers within 24 hours of surgery.
What is the recovery like?
Septoplasty Recovery
 Healing is a slow and gradual process that requires patience and care. Cartilage may require up to a year to fully settle into its new shape. After a septoplasty, a person’s nose may be packed with cotton to keep the new and improved nasal airway patent. You can expect swelling and some bruising after surgery that will begin to improve a couple days after surgery, however, it may last up to two weeks. It is important to remember that the final shape of your nose will not be apparent until after it has completely healed. Strenuous activities, such as intense workouts, running, lifting weights, and contact sports should be avoided for three to six weeks after surgery, because such strenuous activities may result in an increase in blood pressure, which in turn may increase a patient’s chance of bleeding. You may return to your social activities as soon as two to three weeks without any recognizable signs that you had a procedure done.
Healing is a slow and gradual process that requires patience and care. Cartilage may require up to a year to fully settle into its new shape. After a septoplasty, a person’s nose may be packed with cotton to keep the new and improved nasal airway patent. You can expect swelling and some bruising after surgery that will begin to improve a couple days after surgery, however, it may last up to two weeks. It is important to remember that the final shape of your nose will not be apparent until after it has completely healed. Strenuous activities, such as intense workouts, running, lifting weights, and contact sports should be avoided for three to six weeks after surgery, because such strenuous activities may result in an increase in blood pressure, which in turn may increase a patient’s chance of bleeding. You may return to your social activities as soon as two to three weeks without any recognizable signs that you had a procedure done.
As part of your septoplasty recovery, you may have a “nasal drip pad” placed under your nostrils to collect any blood that may drip from your nose. The nurse will show you how to properly place and remove the drip pade so that you may take care of it at home. Packing and the nasal drip pad will be removed within 2-3 days after surgery by your surgeon at your follow-up appointment. Your nose may feel stuffy or congested and you may have trouble breathing for a short time. The skin on the tip of your nose may be numb. You may notice itching and/or an increase in pain intensity as the anesthesia wears off and the feeling returns to your nose. While initial swelling subsides within a few weeks, it may take up to a year for your new nasal contour to fully refine. During this time you may notice gradual changes in the appearance of your nose as it refines to its permanent outcome.
Activity
- Rest as much as possible, getting adequate sleep will help you recover.
- Keep your head raised for several days after surgery. Sleep with your head elevated by using 2 or 3 pillows.
- Try to walk each day and slowly increase the amount you walk daily.
- Take a week off from work. Necessary time off varies depending on the type of work you do and how you feel, but it is important that you take the time to rest and allow your body to recover.
- Avoid strenuous activities, such as bicycle riding, jogging, weight lifting, running or aerobic exercise, for 2 to 3 weeks or until your doctor says it is okay.
- Do not blow your nose for at least 3-5 days after surgery. Dab your nose gently with a tissue. If you need to sneeze, sneeze with your mouth open.
- Avoid bending over.
- Do not rub your nose for 8 weeks. Use sunblock on your nose and wear a hat with a brim to avoid getting sunburn. Put on sunblock or makeup gently.
- No swimming for 1 week.
Diet
- It is common for your bowel movements to be slowed or slightly irregular following your surgery and that may be a result of the medications you are given while under anesthesia.
- Avoid straining with bowel movements. You may want to take a fiber supplement to help with constipation. If you have not had a bowel movement after a couple of days, contact your doctor and ask about taking a mild laxative.
Medicines
- Your doctor will tell you if and when you can restart your usual regimen of medications, as well as when you can begin your new prescription of medications provided to you after the surgery.
- If you take blood thinners, such as warfarin (Coumadin), clopidogrel (Plavix), or aspirin, your provider will tell you if and when to start taking those medicines again.
- Take pain medicines exactly as directed on your prescription.
- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better, it is important that you take the full course of your antibiotics.
Incision care
- After the stitches are out, you may wash the incision with gentle soap and water and gently pat the area dry.
Other instructions
-
- Put ice or a cold pack on your nose for 10 to 20 minutes at a time, every 1 to 2 hours for 3 days (when awake) or until the swelling goes down.
- Do not set glasses on your nose for 4 weeks.
- For 1 week, avoid wearing clothes that you have to pull over your head, as this may cause trauma to your nose.
How long does it take?
A septoplasty is an outpatient procedure that generally takes anywhere from 30 to 90 minutes. As with any surgery, the length of time of a septoplasty surgery varies from person to person.
REASONS THAT AFFECT SURGERY TIME
- Minimal changes will generally take about an hour to an hour and a half. If there are more extensive changes taking place, then the surgery could last up to 2 hours.
- The amount of cartilage that needs to be removed to achieve optimal results could add to or lessen the overall surgery time.
- If you have breathing issues that need to be addressed, the surgery can take longer.
- The reason for the surgery; the septoplasty time length will vary depending upon what caused the trauma or damage to the cartilage and how extensive it is.
How long has it been around?

Septoplasties began increasing in popularity in 1757 when Dr. Quelmatz became one of the earliest physicians to address septal deformities. In the late 19th century, the most common operation in the United States was the Bosworth operation, which was used to correct nasal obstructions caused by nasal septal deviation. Surgeons used a specialized saw to remove the deviation along with the corresponding mucosa, leaving patients with suboptimal results. Dr. Ingals is credited as the father of modern septal surgery, as he innovated this procedure by introducing en bloc resection of small sections of septal cartilage. Around the same time, anesthesia and hemostasis for nasal surgery was improving dramatically, making longer and more technically refined operations feasible. Practices continued to improve and were revised with time, advancing septoplasties to be what we know of today.
What are the complications?
What are the risks of septoplasty?
With all procedures, there are benefits and risks, and it is up to you to decide if the benefits outweigh the risks, or vice versa. Your plastic surgeon and/or staff will explain in detail the risks associated with surgery. You will be asked to sign consent forms to ensure that you fully understand the procedure and any risks or potential complications. It is also important that patients go into the procedure with realistic expectations.
Septoplasty surgery risks include:
- Anesthesia risks
- Infection
- Poor wound healing or scarring
- Change in skin sensation (numbness or pain)
- Altered nose shape
- Difficulty breathing
- Unsatisfactory nasal appearance
- Skin discoloration and swelling
- Decreased sense of smell
- Nasal septal perforation (a hole in the nasal septum) which is rare. Additional surgical treatment may be necessary to repair the septum but it may be impossible to correct this complication.
These risks and others will be fully discussed prior to your consent. It is important that you address all your questions directly with your plastic surgeon.
What can you do to speed up recovery?
It is important that patients practice patience and remember that the recovery process takes time. During this time, there are steps you can take to speed things up and ensure that everything heals properly.
Septoplasty Recovery Timeline
The average Septoplasty recovery time is about one year, but it varies with each individual. That may sound like a long time, but when it’s broken down into a timeline, it is easier to understand. The following recovery milestones may vary from patient to patient:
1 Week: The packing and dressing will be removed within this time and you can go out in public without showing noticeable signs of surgery unless there is bruising around the eyes. This may take 2 weeks to resolve. It is safe to resume activities of daily living.
2 Weeks: The majority of the swelling, if any has subsided and most of the bruising should have resolved.
3-4 Weeks: You can safely return to cardiovascular activities such as jogging, swimming and cycling.
6 Weeks: The bones are stable; you can resume resistance workouts (weight lifting), wearing glasses and blowing your nose.
3-6 months: The numbness and abnormal sensations in your nose and nasal skin should be resolved.
1 Year: The healing process is complete – the cartilage should have fully settled and swelling should have subsided entirely as the nose’s new shape is fully refined.
Listen to Your Doctor
First and foremost, follow your doctor’s instructions. You will receive specific instructions on what medications to take, when to take them, how to care for the surgical site to prevent infection, and when you’ll need to come back in for a follow-up exam.
Listen to Your Body
Your plastic surgeon will be able to see how your septoplasty recovery is going from the outside, but only you will know how you’re feeling. Listen to your body – if something doesn’t feel right after surgery, discuss it with your doctor right away.
Keep Your Head Elevated
Sleeping on your side after septoplasty isn’t just uncomfortable – it can prolong your recovery time by causing additional bruising and swelling. You’ll need to keep your head elevated at night for 6 weeks following surgery. Prop your head up on two or three pillows or use a foam wedge when you sleep or sleep in a recliner.
Use Cold Compresses
In the first 72 hours after surgery, using a cold compress can help significantly reduce swelling. Just be careful not to apply the compress directly to your nose. Instead, apply it to your cheeks so that you don’t accidentally shift any bones or cartilage.
Get Plenty of Rest
The congestion you feel after surgery may make it more difficult to fall asleep, but rest is a vital part of the recovery process. Your body uses energy to heal itself, and getting a solid seven or eight hours of sleep each night gives your body time to restore that energy.
Maintain a Healthy Diet
Eating a balanced diet post-surgery can help to speed up your recovery by giving your body the nutrients it needs to heal itself. A diet consisting of nuts, meat, eggs, yogurt, fish, and other protein-rich foods will help your body rebuild the damaged tissue in and around your nose. You’ll also want to make sure you’re getting plenty of vitamins in your diet, namely Vitamin A and Vitamin C.
Stay Cool
Steamy showers, hot bowls of soup, and relaxing saunas will not benefit you after the procedure. Heat will cause the tissues in your nose to swell even more, which is why it’s best to stick to a diet of cool and room-temperature foods, take lukewarm showers, and stay out of the heat in the weeks following your nose reshaping procedure.
Don’t Blow Your Nose
After surgery, you’re going to experience some congestion for a few weeks, maybe even a few months. This feeling is caused by swollen nasal tissues. Resist the urge to blow your nose and talk with your doctor about using a saline nasal spray to gently moisturize your nasal passages until the swelling goes down. You may resume blowing your nose about 6 weeks after surgery.
Avoid Vigorous Exercise
Iit takes time for you to heal and it is necessary you avoid strenuous exercise. Movements that seem harmless like stretching, lifting, or bending over can increase nasal swelling. Additionally, strenuous exercise and activity may increase your blood pressure, making you more prone to bleeding. Wait until your doctor approves of you advancing to your normal activity.
Don’t Wear Glasses
Sunglasses, reading glasses, prescription glasses – anything that puts pressure on your nose as it’s healing can cause additional bruising or swelling. Your facial plastic surgeon will advise you on when it’s safe to start wearing glasses again. In the meantime, switch to contacts, if you can.
Stay Out of the Sun
It’s always a good idea to protect your skin from getting too much sun exposure, but this is especially important after surgery. Not only is your nose more prone to sunburn in the weeks and months following the procedure, but too much sun can also cause any scarring you have to darken and swelling to increase.
Avoid Aspirin
Don’t be tempted to use aspirin as a painkiller. It thins the blood, and this can make bleeding more likely and prevent blood clotting that is needed to speed up recovery. For this reason, aspirin should be avoided for two weeks before and after surgery. Vitamin E supplements and Ibuprofen and Motrin should also be avoided for the same reason.
Do you need to rest up afterwards and for how many days?
Everyone heals differently and has unique requirements to aid them in their recovery. Below is a general guideline for what a person may expect in the weeks to come and how much rest they should allow themselves.
1-5 days post-surgery
Resting, icing, and hydrating is most important immediately after the procedure to speed up recovery.
Over these first few days, blowing your nose could open your incisions, so don’t risk it. You might also have a slight headache. Aspirin or ibuprofen will increase your bleeding risk, so avoid those medications and follow the prescription of pain medications given to by your surgeon, if you feel like you need them. Keep in mind that such pain medications have the potential to make you constipated, so make sure you increase your fiber and talk to your surgeon about the use of laxatives. Your doctor will recommend using small, light ice packs on your eyes and cheeks for 15 minutes every hour, to reduce swelling, just remember to avoid putting too much pressure on your nose.
1 week post-surgery
Between five to seven days after surgery, your surgeon should remove the packing and dressing and you’ll get your first look at your new nose. You shouldn’t require as much rest during this time. Keep in mind that the swelling is still going down and your final result will take time, and may even look different than what you are initially seeing.
1-2 weeks post-surgery
Head back to work
Once your dressing is off and the packing is removed and the worst of your swelling has gone down, you could head back to work, with makeup over your bruises. If you want to be really discreet, you may want to wait up to two weeks for the swelling to go down.
2-3 weeks post-surgery
If you have glasses, you can wear them normally again.
Glasses can put pressure on the bridge or the sidewalls of your nose, which can complicate healing and feel really uncomfortable. In the next few weeks, you may be able to start wearing glasses again for short periods, with frequent breaks.
3-6 weeks post-surgery
Start exercising again
In the first few weeks, exercise could increase your blood pressure to a point beyond what’s healthy for your healing tissues.
You should follow your surgeon’s recommendations on physical activity and exercising. It is important to avoid any strenuous activity or exercise that increases blood pressure for the first two to three weeks post surgery.
For 3 months post-surgery
Keep your nose protected from trauma
It’s especially important to avoid any accidental bumps during these first three months of healing, when it’s more vulnerable.
6 months post-op
Expect your nasal swelling to be almost gone
At this point, your swelling should have dramatically subsided. Keep in mind that things are still healing and settling, so you won’t see your final results for another six months, at least.
1 year post-septoplasty
Evaluate your final results
Most people will be able to assess their final results a year after their septoplasty. It takes at least this long for your cartilage to fully settle and it is important to be patient!
